The management of diabetes is undergoing a transformation, thanks to advancements in technology and the development of smart insulin pumps. These devices are not just about delivering insulin; they’re about enhancing the quality of life for individuals with diabetes through precise, automated control of blood glucose levels.
This guide explores how smart insulin pumps are revolutionizing diabetes care, offering newfound freedom and tighter glucose control than ever before.
The Evolution of Insulin Delivery
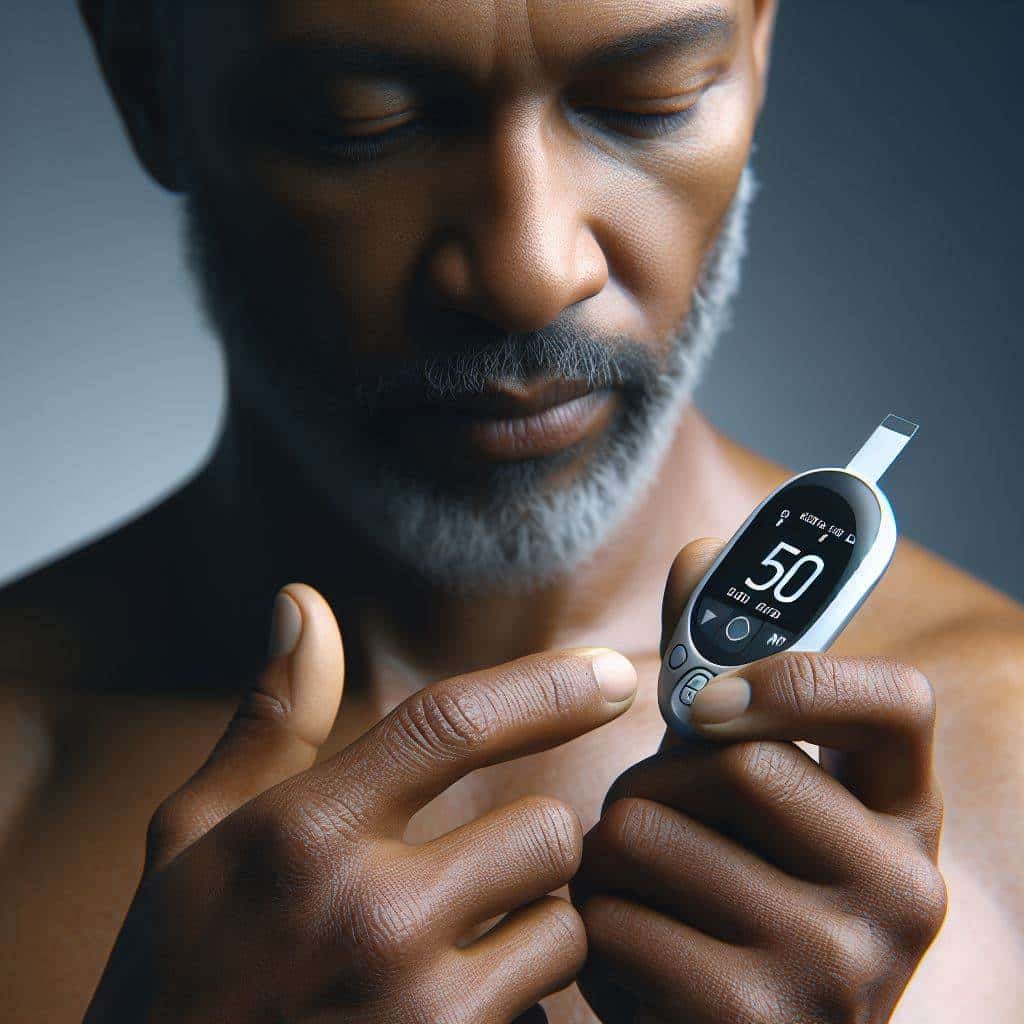
Insulin therapy has evolved significantly since its discovery, moving from syringes and vials to pen injectors and, most recently, to insulin pumps. Smart insulin pumps represent the latest innovation, integrating continuous glucose monitoring (CGM) data to automate insulin delivery. This technology aims to mimic the pancreas’s natural insulin release, reducing the burden of manual glucose management.
- Increased Accuracy: Smart pumps adjust insulin doses based on real-time glucose readings.
- Enhanced Convenience: The integration with CGM devices means fewer finger pricks and manual injections.
- Personalized Care: Algorithms can be tailored to an individual’s unique insulin needs and lifestyle.
Benefits of Smart Insulin Pumps
Smart insulin pumps offer several benefits over traditional insulin delivery methods, improving both clinical outcomes and user experience.
- Tighter Glucose Control: By continuously adjusting insulin delivery, smart pumps can maintain glucose levels within a tighter range, reducing the risk of both hyperglycemia and hypoglycemia.
- Reduced Diabetes Management Burden: The automation of insulin dosing relieves users from constant decision-making and manual adjustments.
- Improved Quality of Life: Users often report greater satisfaction and a sense of normalcy, as smart pumps allow for more flexibility in daily activities and diet.
- Data-Driven Insights: The integration with CGM provides valuable data for users and healthcare providers, enabling more informed treatment decisions.
Integrating Smart Pumps into Your Diabetes Care Plan
Integrating smart insulin pumps into your diabetes care plan marks a pivotal step toward enhanced management and autonomy over your health. Smart pumps, with their advanced features and continuous glucose monitoring (CGM) integration, offer a dynamic approach to controlling blood sugar levels. However, transitioning to this sophisticated technology requires a structured approach, encompassing consultation, education, and an adjustment period to ensure its success.
Consultation with a Diabetes Care Team
The journey to adopting a smart insulin pump begins with a thorough consultation with your diabetes care team. This multidisciplinary team, often including endocrinologists, diabetes educators, and nurses, will evaluate your suitability for a smart pump. Factors such as the type and stability of your diabetes, your lifestyle habits, and your specific treatment objectives will be assessed. This step is crucial not only for determining if a smart pump is right for you but also for tailoring the technology to meet your individual needs. It’s an opportunity to discuss how a smart pump could fit into your daily routine and address any concerns you may have about making the switch.
Training and Education
Once a decision has been made to proceed with a smart insulin pump, comprehensive training and education are essential. Learning how to operate the pump is just the beginning. You’ll also need to become proficient in interpreting the data provided by the CGM, understanding how different activities and foods affect your glucose levels, and knowing how to adjust your insulin doses accordingly. Training may cover how to respond effectively to the pump’s alerts and alarms, which are designed to notify you of potential issues such as low or high blood sugar levels. Many manufacturers and diabetes care teams offer detailed training sessions and resources to help new users feel confident and informed.
Adjustment Period
Transitioning to a smart insulin pump is not without its challenges, and there is often an adjustment period as you learn to trust and rely on the device. During this time, it’s common to fine-tune the pump’s settings and features to better match your body’s insulin needs. This period of customization is critical for optimizing the pump’s effectiveness and requires ongoing communication with your diabetes care team. Regular follow-up appointments allow for the assessment of your progress, the addressing of any issues, and the making of necessary adjustments to your treatment plan. It’s also a time for personal reflection on how the pump is impacting your life, allowing for adjustments not just to the device’s settings but also to your expectations and daily routines.
Embracing the Change
Adopting a smart insulin pump is a significant change that can vastly improve the quality of life for many people with diabetes. It offers the promise of tighter glucose control, reduced risk of complications, and a more flexible lifestyle. However, success with a smart pump is built on a foundation of thorough preparation, continuous learning, and open communication with your healthcare providers. By embracing these steps, you can ensure a smooth transition and make the most of what smart insulin technology has to offer in diabetes management.
| Model Name | Manufacturer | Wearable Duration | Connectivity | Integration with CGM | Key Features |
|---|---|---|---|---|---|
| MiniMed 780G | Medtronic | Up to 7 days | Bluetooth, Smartphone App | Yes, compatible with Guardian Sensor 4 | Advanced hybrid closed-loop system, customizable glucose targets |
| Tandem t:slim X2 | Tandem Diabetes Care | Up to 10 days | Bluetooth, t:connect mobile app | Yes, Dexcom G6 integration | Control-IQ technology, touchscreen interface |
| Omnipod 5 | Insulet Corporation | Up to 3 days (72 hours) | Bluetooth, Omnipod 5 App | Yes, Dexcom G6 integration | Tubeless design, automated insulin delivery |
Wearable Duration explanation
“Wearable duration” refers to the length of time a medical device, such as a smart insulin pump or a continuous glucose monitoring (CGM) sensor, can be worn on the body before it needs to be replaced or removed. This term is particularly relevant for devices that are applied directly to the skin and have a finite operational lifespan due to factors like battery life, adhesive wear, sensor accuracy degradation, or reservoir capacity for insulin pumps.
For insulin pumps, wearable duration might specifically refer to how long the infusion set (the part that delivers insulin from the pump into the body) can stay inserted in the skin before it needs to be changed to a new site to prevent infection or irritation.
For CGM sensors, wearable duration indicates how long the sensor can accurately measure glucose levels before it must be replaced. This period can vary widely depending on the technology and manufacturer’s design, ranging from several days to up to two weeks or more.
Understanding the wearable duration of these devices is crucial for users as it impacts the management routine, the cost of supplies, and the overall user experience with the device. Longer wearable durations can offer more convenience and potentially lower the burden of managing diabetes, but they must be balanced with the need for maintaining skin health and ensuring the accuracy and efficacy of the device.
Navigating Challenges and Considerations
Navigating the challenges and considerations associated with smart insulin pumps is an integral part of integrating these advanced devices into your diabetes management plan. While smart pumps offer a revolutionary approach to managing blood glucose levels, users may encounter several hurdles that can impact their experience. Understanding these challenges and adopting effective strategies to overcome them is crucial for maximizing the benefits of smart insulin pump technology.
Dealing with Device Malfunctions
One of the primary concerns for smart insulin pump users is the possibility of device malfunctions. These can range from sensor inaccuracies to complete device failures. To mitigate these issues, it’s essential to have a comprehensive understanding of your device’s operation and maintenance requirements. Thorough training provided by healthcare professionals or the device manufacturer can equip you with the knowledge to troubleshoot common problems and recognize when professional assistance is needed. Additionally, maintaining regular communication with the device manufacturer for software updates and technical support can help prevent malfunctions and ensure your pump is functioning optimally.
Managing Insertion Site Infections
Insertion site infections are a potential risk associated with the continuous use of insulin pump infusion sets. Proper site care is paramount to preventing infections. This includes rotating the infusion site with each new set, cleaning the skin thoroughly before insertion, and monitoring the site for signs of irritation or infection. If an infection is suspected, it’s important to consult with your healthcare provider immediately to receive appropriate treatment. Educating yourself on best practices for site care and hygiene can significantly reduce the risk of infections and enhance your overall experience with the pump.
Addressing Insurance Coverage and Costs
The cost of smart insulin pumps and ongoing supplies, such as infusion sets and sensors, can be significant. Insurance coverage varies widely and may not fully cover the expenses associated with pump therapy. Navigating insurance coverage requires a proactive approach: understanding your insurance policy, communicating with your insurance provider to clarify what is covered, and advocating for the necessary coverage. In some cases, assistance programs offered by pump manufacturers or third-party organizations may help offset costs. Preparing documentation that demonstrates the medical necessity of a smart insulin pump, such as records of blood glucose logs or letters from your healthcare provider, can strengthen your case for insurance coverage.
Embracing Support and Resources
Overcoming the challenges associated with smart insulin pumps often involves leveraging support and resources from a variety of sources. Joining diabetes support groups, either in-person or online, can provide valuable insights and tips from other pump users. Healthcare teams, including diabetes educators and endocrinologists, are essential resources for personalized advice and problem-solving strategies. Additionally, manufacturers often provide educational materials, training sessions, and customer support to assist with technical issues and usage questions.
Navigating the challenges of smart insulin pump therapy requires a combination of knowledge, preparation, and support. By understanding potential obstacles and implementing effective strategies to address them, users can enhance their experience and achieve better outcomes with their diabetes management.
Smart Insulin Pumps for Diabetes: Your FAQs Answered
What is a smart insulin pump?
A smart insulin pump is a device that automates insulin delivery, adjusting the dose based on continuous glucose monitoring (CGM) data to better manage blood glucose levels.
How do smart insulin pumps differ from traditional pumps?
Unlike traditional pumps, smart pumps use algorithms to automatically adjust insulin delivery based on real-time CGM data, reducing the need for manual adjustments.
Can anyone with diabetes use a smart insulin pump?
Smart insulin pumps are typically recommended for individuals with type 1 diabetes and some cases of type 2 diabetes requiring intensive insulin therapy. A healthcare provider can assess suitability.
Are smart insulin pumps covered by insurance?
Coverage varies by insurance plan and location. Many insurance providers cover smart insulin pumps under certain conditions, but pre-approval and documentation of diabetes management needs may be required.
How can a smart insulin pump improve diabetes management?
By continuously adjusting insulin doses based on glucose levels, smart pumps can help maintain tighter glucose control, reduce the risk of hypoglycemia and hyperglycemia, and alleviate the daily management burden.
What should I consider before choosing a smart insulin pump?
Consider factors like the pump’s compatibility with CGM systems, the need for calibration, battery life, insulin reservoir capacity, and personal lifestyle needs.
How often do I need to interact with my smart insulin pump?
While smart pumps automate insulin delivery, users still need to input mealtime carbohydrates, monitor CGM data, and respond to alerts. Regular interaction is necessary for optimal performance.
Can I swim or shower with my smart insulin pump?
Many smart insulin pumps are water-resistant, allowing for brief exposure to water. However, it’s important to check the manufacturer’s guidelines regarding depth and duration limits.
What are the common challenges with using a smart insulin pump?
Challenges can include managing insertion site infections, dealing with adhesive allergies, learning to trust the device’s automation, and navigating technical issues or malfunctions.
How do I start using a smart insulin pump?
Starting with a smart insulin pump involves consulting with your diabetes care team, undergoing training on using the pump and CGM system, and gradually adjusting to the device as part of your diabetes care regimen.
Citations
- Bergenstal, R. M., et al. (2010). “Threshold-Based Insulin-Pump Interruption for Reduction of Hypoglycemia.” The New England Journal of Medicine, 363(4), 311-320. This landmark study examines the efficacy of threshold-based insulin pump interruption in reducing the incidence of hypoglycemia in patients with type 1 diabetes.
- Pickup, J. C., & Sutton, A. J. (2008). “Severe hypoglycaemia and glycaemic control in Type 1 diabetes: Meta-analysis of multiple daily insulin injections compared with continuous subcutaneous insulin infusion.” Diabetic Medicine, 25(7), 765-774. This meta-analysis compares the outcomes of multiple daily injections versus continuous subcutaneous insulin infusion (CSII), or insulin pump therapy, highlighting the impact on glycemic control and risk of hypoglycemia.
- Weinzimer, S. A., et al. (2008). “Effectiveness of Continuous Glucose Monitoring in a Clinical Care Environment: Evidence from the Juvenile Diabetes Research Foundation Continuous Glucose Monitoring (JDRF-CGM) Trial.” Diabetes Care, 31(1), 17-22. This trial assesses the effectiveness of continuous glucose monitoring systems in improving glycemic control in various age groups within a clinical care setting.
- Garg, S. K., et al. (2017). “Glucose Outcomes with the In-Home Use of a Hybrid Closed-Loop Insulin Delivery System in Adolescents and Adults with Type 1 Diabetes.” Diabetes Technology & Therapeutics, 19(3), 155-163. The study evaluates the in-home use of a hybrid closed-loop system, examining its impact on glucose control in individuals with type 1 diabetes.